Transform Population OutcomesWith Real-Time Intelligence
Manage 125K+ member populations with AI-powered risk stratification, predictive analytics, and automated care coordination. Built for federal healthcare scale.
Real-Time Population Analytics
Monitor your entire population's health with intuitive dashboards and actionable insights
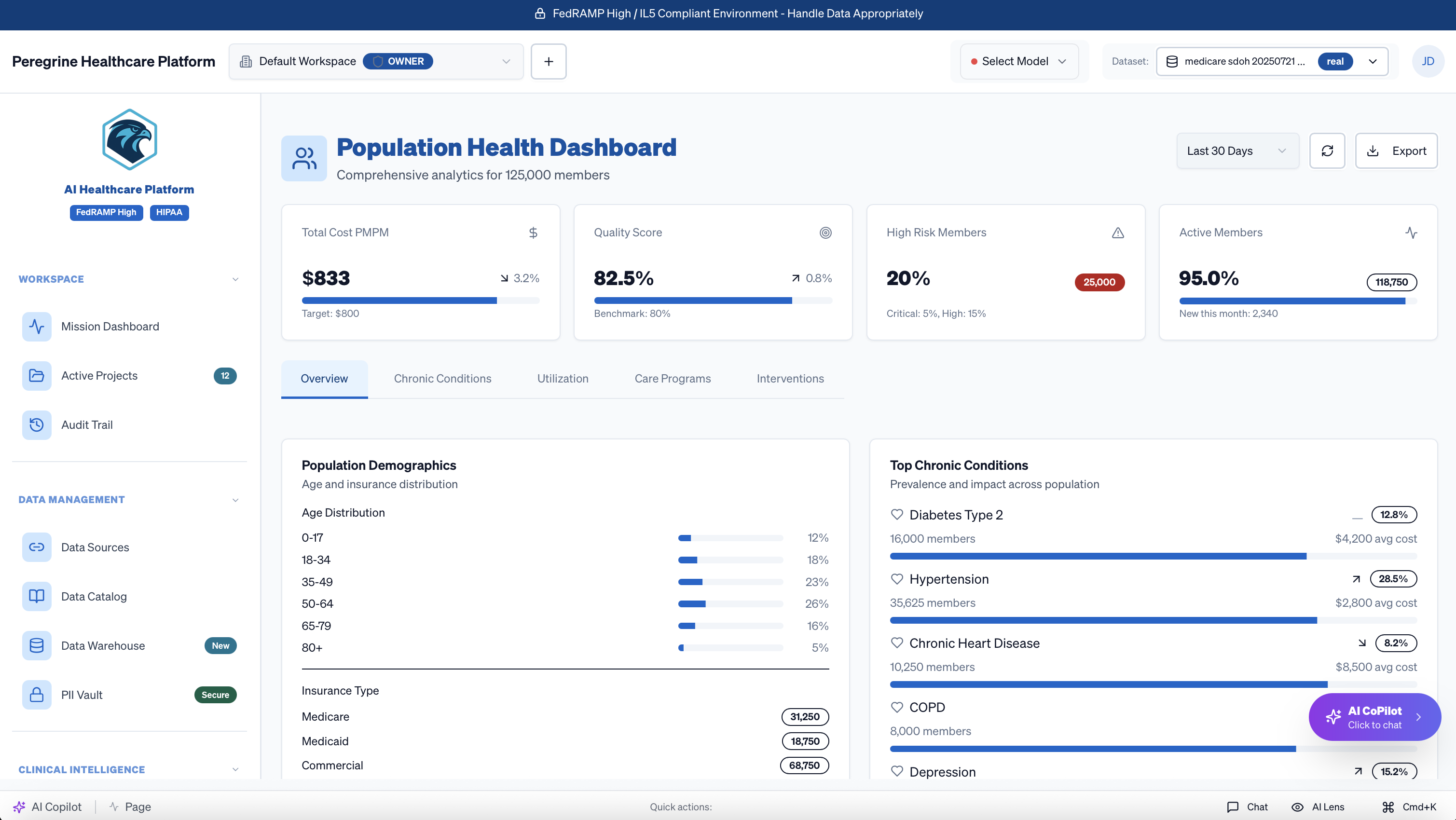
Click to explore the population health dashboard
Comprehensive Population Management
Everything you need to improve outcomes and reduce costs across your entire population
Risk Stratification
AI-powered risk models identify high-risk members before acute events
- Predictive readmission models
- Chronic disease progression
- Social determinant impacts
- Cost prediction algorithms
Care Gap Analysis
Automatically identify and prioritize care gaps across quality measures
- HEDIS gap identification
- Star ratings optimization
- Preventive care tracking
- Custom measure support
Care Coordination
Streamline care team collaboration with automated workflows
- Care team assignments
- Task management
- Automated outreach
- Progress tracking
Performance Analytics
Deep insights into program effectiveness and ROI
- Quality measure trends
- Cost analysis
- Utilization patterns
- Benchmark comparisons
Real-time Monitoring
Track population health metrics as they happen
- ADT feed integration
- ER visit alerts
- Admission notifications
- Discharge follow-up
Intervention Management
Design and track targeted interventions for at-risk cohorts
- Campaign builder
- A/B testing
- Outcome tracking
- ROI measurement
Advanced Risk Stratification
Our AI models analyze 200+ factors to predict risk with unprecedented accuracy
Multi-Dimensional Risk Scoring
Clinical Risk Factors
Social Determinants
Utilization Patterns
Behavioral Indicators
Risk Score Distribution
Immediate intervention required
Preventive care focus
Routine monitoring
Wellness programs
Proven Outcomes & ROI
Real results from healthcare organizations using our population health platform
Clinical Outcomes
Financial Impact
Time to Value
Most organizations see measurable improvements within 90 days
30 days
Initial insights
60 days
First interventions
90 days
Measurable ROI
Seamless Data Integration
Connect all your data sources for a complete view of population health
Clinical Data
- • EHR/EMR systems
- • Lab results
- • Pharmacy data
- • ADT feeds
Claims & Financial
- • Medical claims
- • Pharmacy claims
- • Eligibility files
- • Risk adjustment
External Sources
- • HIE data
- • SDoH databases
- • Public health registries
- • Wearable devices
Ready to Transform Your Population's Health?
Join leading healthcare organizations achieving breakthrough outcomes